
You’ve heard this before, but I’ll say it again - telehealth is taking off around the world. In Canada, we lag behind some of the leading nations in health care technology, so maybe we don’t quite have a sense of how fast things are happening. For a reality check, consider that in 2016, Kaiser Permanente (the largest integrated health network in the US) conducted more virtual consultations than in person – 52% of 110 million visits were completed with online portals, virtual visits, or apps.1
Physiotherapy is participating in this growth, even in our own province. Locally, there are examples of telerehabilitation programs for stroke rehabilitation, musculoskeletal assessment and treatment, employer-funded consultations for remote workers, and more. Joint replacement telerehabilitation could be on the way soon. In all of these cases, the main benefit is improved access. For those whose access was limited by location, cost of travel or by mobility have increased opportunities and can now receive treatment.
As a profession moves into a new form of practice, that growth will be facilitated by common language. This is difficult, when for most of us, digital health is learned by osmosis as we either become interested or are forced into it. Therefore, it is a good time for us as a profession to step back and clarify some terminology. Please read on, as I help to clarify.
A Framework for Tele-Terminology
We exist in a digital health terminology swamp. Digital health, virtual health, telehealth, ehealth, etc. What is the real substance of these words?
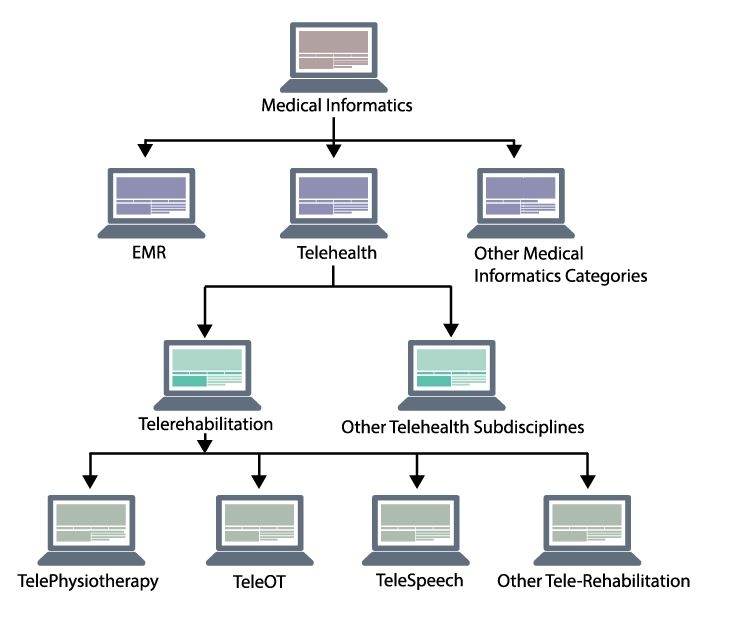
Let’s handle of few of them, particularly the ‘tele’ terms. Generally, the application of the computers to the practice of medicine is, in its broadest sense, referred to as “Medical Informatics”. There are a multitude of categories through which digital meets medical under this broad umbrella, and one of them is “telehealth”. The American Telemedicine Association (ATA), considered a primary global leader in the telehealth landscape, moved from the term “telemedicine” to “telehealth” in 2005 – giving a label to the broadest category of this set of tools and practices.
They have defined telehealth (TH) as: “a broad term used to describe the use of electronic or digital information and communications technologies (ICT) to support clinical healthcare, patient and professional health-related education, and public health administration”.2
There are at least three things worth noting here. Firstly, the prefix “tele” literally means “at” or “from a distance”. For a practice to be included under the TH umbrella, it typically would be performed between two sites a distance from each other. Secondly, information and communication technologies are used. In modern times this means computers and high-speed data networks. Finally, note that TH is not necessarily patient treatment, it may be the use of ‘tele’ tools to provide health professional education, or even health administration.
The term “telemedicine” continues to be used interchangeably with TH, but the ATA suggests telemedicine has the distinction of being primarily related to the provision of clinical services to improve the health of a specific patient. Telemedicine may have different subcategories itself, such as teledermatology or telecardiology. In the end, telemedicine is a form of TH, but TH is not necessarily telemedicine.
“It is a good time for us as a profession to step back and clarify some terminology.”
So what do we call it when a physiotherapist delivers clinical services through ICT from a remote location? Telehealth? Yep. Telemedicine? You could say that too, but it would be best to be specific. For that, we use the term “Telerehabilitation” (TR). The ATA Telerehabilitation Special Interest Group describes TR as an important subdiscipline of telehealth, and defines it as: “The delivery of rehabilitation and habilitation services via information and communication technologies (ICT), also commonly referred to as “telehealth technologies”. Telerehabilitation can include evaluation, assessment, monitoring, prevention, intervention, supervision, education, consultation and coaching”.2, 3
Notice the broad potential here and realize that TR is not synonymous with videoconferencing. Yes, image-based technologies are the most recognizable and studied form of TR, but to leave it there would be to miss the real potential.
The integration of sensors, virtual reality, and asynchronous technologies are all a part of TR and vastly expand the impact we can have on patients’ lives. Some try to move away from tele-terminology, as it compels images of the telephone. However, I would contest if we rescue the true meaning of “tele” (at, or from a distance), I do believe the definitions provided by the ATA gives the most logical and rich framework for considering the full scope of remote, technology-enabled, rehabilitation practice.
TR practices can theoretically be further specified as telephysiotherapy, tele-speech, TeleOT. Although these terms are still finding their place in practice. What may be more interesting is the various models of care that can be undertaken within telerehabilitation, but we will have to leave that until the next article. For now, hopefully your physiotherapy tele-lexicon has uploaded some new information that will help you in the digital health world.
| References |
|---|
| 1 Owens B. Telemedicine on the rise but lagging in Canada. Can Med Assoc J. 2018;190(38):E1149-E1150. |
| 2. Richmond T, Peterson C, Cason J, et al. American telemedicine association’s principles for delivering telerehabilitation services. International Journal of Telerehabilitation. 2017;9(2):63-68. |
| 3. Kumar S, Cohn, Ellen R (Speech therapist), SpringerLink ebooks - Medicine. Telerehabilitation. London; New York: Springer; 2012. |
Jeremy McAllister, BScPT, MHA
PABC eHealth Manager
Featured Article in PABC Directions, Spring 2019 Edition